김혜성 이사장(서울치대 졸업, 동대학원 박사)
사과나무의료재단의 이사장이자, 재단 산하 의생명연구소의 미생물 연구자이다.
구강미생물에서 시작해 장내 미생물, 발효 음식의 미생물까지 폭넓게 공부하며 몇 권의 책을 냈고 논문을 발표했다.
『미생물과의 공존』 『입속에서 시작하는 미생물이야기』 『미생물과 공존하는 나는 통생명체다』등 3권이 과학기술부 선정 우수과학도서를 수상했다.
구글에 ‘floss or die’란 캠페인성 문구가 보입니다. ‘치실을 쓸래 죽을래…’라고 너무 직접적으로 들이대는 듯하지만, 그만큼 치간관리의 중요성을 강조하는 듯합니다. 참 간단해 보이는 아이디어인데도, 이미 1815년에 개발이 되고, 1898년에 첫 특허까지 낸 치실은, 오랫동안 치간사이 음식물을 제거하는 역할을 해 온 듯합니다.(https://www.oralhealthgroup.com/features/gum-disease-starts-teeth/)
저 역시 늘 주머니에 치실이 들어있고 없으면 불안해 가까운 편의점에서 사는 경우도 많습니다. 치간 사이에 음식이 껴서 잇몸이 눌리면 얼마나 신경쓰이고 불편한지는 겪어보지 않으면 알지 못할 겁니다.
그렇더라도, 실제로 치실이 치간사이의 플라크를 제거하는 역할은 크지 않아 보입니다. 음식물 제거 효과는 크겠지만요. 2015년의 메타분석 논문을 포함한 여러 평가에서도, 치실은, 플라크 제거에 그다지 효율적이지 않다 지적합니다.(Sälzer, Slot et al. 2015) 실제 쓰는 것도 쉽지 않기도 하지요. 그래서인지, 오래된 역사에도 불구하고, 저처럼 치실을 늘 쓰는 사람은 채 30%도 되지 않는다고 합니다.
그래도, floss or die가 전하는 메시지는 분명합니다. 치간관리(interdental space)가 참 중요하다는 거죠. 일상의 칫솔질로는 치간사이가 관리되지 않음은 분명하니까요. 해부학적으로 보면 상당히 복잡한 치간의 모양은 그래서 플라크가 잘 끼고, 치주질환이 가장 먼저 시작되는 곳이기도 합니다. 통계적으론, 몇 % 의 치주질환이 치간에서 시작되는지는 검색되지 않지만, 거의 대부분의 치주질환이 치간에서 시작된다는 추정은 일리가 있어 보입니다. 진료실에서도, 치주포켓의 깊이를 재 볼 때도 치간으로 먼저 손이 가는 것도 당연해 보이고요.
현재까지 치간 사이의 관리에 가장 효율적이라 평가받는 것은, 당연히 치간칫솔(interdental brush) 입니다. 1976년에 처음 시장에 등장한 치간칫솔은, 이제 편의점에 1회용 치간칫솔이 전시되어 있을 만큼 일상화되어 가고 있습니다.
치간칫솔은 치은연(gingival margin) 2~2.5 mm 하방의 플라크까지도 잘 제거하여 치간관리에 유효함을 보여줍니다.(Waerhaug 1976) 2015년에 있었던 유럽 치주학 연맹(European Federation of Periodontology)은 치간칫솔의 세정효과가 치실이나 이쑤시개에 비해 가장 탁월하고 효과적이라 평가합니다.(Chapple, Van der Weijden et al. 2015)
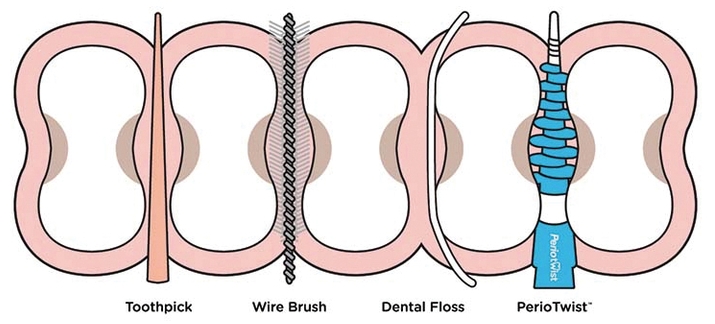
그간 논문을 종합평가한 리뷰논문에서도, 치간칫솔은 플라크 제거나 잇몸출혈, 치주포켓의 감소에 좋은 효과를 낸다고 평가받습니다. 다만, 젊은 사람들 중 치간이 완전히 차 있거나, 동일한 구강 내라도 치간이 열려 있는 곳과 닫혀 있는 곳이 있어서 잇몸자극 등으로 오히려 염증을 일으킬 가능성이 있어서 적절한 대상과 사용위치, 사이즈의 선택 등이 중요할 듯합니다.
제가 최근에 주목하고 있는 것은 구강세정기(oral irrigator) 입니다. 1962년에 시장에 등장한 이 구강세정기는 전기 펄스를 이용한 물 세정으로 치아사이를 닦아냅니다. 이 세정기는 치아사이의 음식물, 플라크 등을 제거할 뿐 아니라, 치주포켓의 깊이가 6mm 정도까지 깊이에도 바이오필름 세정효과를 나타냅니다.(Braun and Ciancio 1992)
또 무엇보다, 이 구강세정기의 효과가 돋보이는 부분은 잇몸의 염증을 낮추어 준다는 겁니다. 치주질환이 있는 환자들에게 구강세정기를 쓰게 했더니, 잇몸염증이 감소하고, 분자적으로도 IL-1β and PGE2 같은 염증성 사이토카인이 감소한 것이 관찰됩니다.(Cutler, Stanford et al. 2000) 저 역시 구강세정기를 늘 사용하는데, 물의 펄스가 잇몸을 자극하는 마사지 느낌이 참 좋습니다. 구강세정기가 혈액순환을 원활히 해줌으로써 염증감소 효과를 나타낼 거라 생각하고 있습니다.
환자들의 지속관리에서 제가 가장 곤란함을 느끼는 경우는 임플란트 주위염입니다. 임플란트 주위염은, 잘 알려져 있다시피, 유전자를 포함해 여러 요인에 의해 생길 수 있지만, 가장 중요한 원인은 역시 구강 내 미생물, 바이오필름의 침착입니다.(Prathapachandran and Suresh 2012) 임플란트 주위염 역시 치간에서 당연히 시작되는 경우가 많고요. 그렇더라도, 선천적으로 갖고 태어난 자연치아에 치주질환이 생기면, 그것을 관리 못한 환자책임인 것이 분명하지만, 왠지 제가 시술한 임플란트에 염증이 생기면 저의 탓 같은 책임감이 더 옵니다.
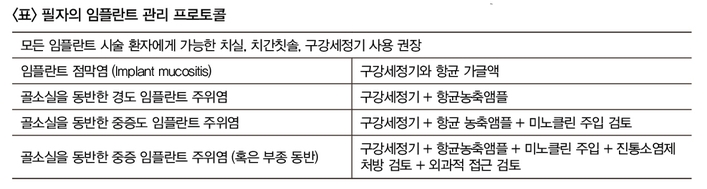
이럴 때, 전 구강세정기를 꼭 권합니다. 임플란트 주위염의 정도에 따라 구강세정기에 항균용액을 타서 쓰는 구강앰플을 처방하기도 하고, 더 심하면 임플란트 주위에 미노클린 연고를 넣고, 부종까지 생겨온 경우, 국소적인 미노클린(minocline) 주입과 함께, 소염제를 경구용으로 처방하기도 합니다.(Heo, Kim et al. 2018) 임플란트 주위염을 비외과적으로 대하는 저의 프로토콜을 표로 정리하면 위의 표처럼 될 듯합니다.
부끄럽지만, 제 입 안에도 임플란트가 여러 개 시술되어 있는 상태입니다. 생물학(자연치아) + 치의학(임플란트)가 결합된 일종의 혼합치열(mixed dentition)이라 할 수 있겠네요.
유치와 영구치가 혼합된 혼합치열이란 용어가, 앞으론 임플란트와 자연치가 혼재된 것을 가리킬지도 모르겠습니다. 임플란트 시술환자가 점점 늘어가고 있고, 노령화와 함께 점점 늘 테니까요. 실제로 2007년 3%에 불과했던 임플란트 장착자율은 2015년 15%까지 늘었고, 이후 노인임플란트 보험화가 되었으니 더욱 늘었을 겁니다.
갈수록 늘어가는 임플란트와 자연치아의 혼합치열에서 가장 불편한 점은 모두 알다시피, 임플란트 주위에 음식물이 낀다는 겁니다. 자연치아의 이동(migration)으로 인해 불가피한 이 현상을, 여러 보철 제작방법으로 커버해 볼 수 있겠지만, 근본적으로는 처음 시술할 때부터 음식물이 낄 것을 예고하고, 치간관리에 신경 써야 함을 확실히 고지시키는 것이 더 중요하고 필요한 일이 아닐까 싶습니다.
치간관리를 잘하는 것은 음식만이 아니라 치간 세균을 제거하는 일이고, 임플란트만이 아니라 자기치아까지 보살피는 일이니까요.
Braun, R. E. and S. G. Ciancio (1992). "Subgingival delivery by an oral irrigation device." J Periodontol 63(5): 469-472.
Irrigating devices have been incorporated into numerous oral hygiene regimens. Newer types of these devices are designed to deliver irrigating solutions directly into the periodontal pocket. We examined the ability of a powered irrigating device with a soft rubber tip to deliver subgingivally into periodontal pockets. When subgingival irrigation was used, the mean pocket penetration was 90% of the pocket depth (less than or equal to 6 mm) compared to a mean of 21% in the oral rinse group. The irrigation was not uncomfortable to patients.
Chapple, I. L., et al. (2015). "Primary prevention of periodontitis: managing gingivitis." J Clin Periodontol 42 Suppl 16: S71-76.
Periodontitis is a ubiquitous and irreversible inflammatory condition and represents a significant public health burden. Severe periodontitis affects over 11% of adults, is a major cause of tooth loss impacting negatively upon speech, nutrition, quality of life and self-esteem, and has systemic inflammatory consequences. Periodontitis is preventable and treatment leads to reduced rates of tooth loss and improved quality of life. However, successful treatment necessitates behaviour change in patients to address lifestyle risk factors (e.g. smoking) and, most importantly, to attain and sustain high standards of daily plaque removal, lifelong. While mechanical plaque removal remains the bedrock of successful periodontal disease management, in high-risk patients it appears that the critical threshold for plaque accumulation to trigger periodontitis is low, and such patients may benefit from adjunctive agents for primary prevention of periodontitis. AIM: The aims of this working group were to systematically review the evidence for primary prevention of periodontitis by preventing gingivitis via four approaches: 1) the efficacy of mechanical self-administered plaque control regimes; 2) the efficacy of self-administered inter-dental mechanical plaque control; 3) the efficacy of adjunctive chemical plaque control; and 4) anti-inflammatory (sole or adjunctive) approaches. METHODS: Two meta-reviews (mechanical plaque removal) and two traditional systematic reviews (chemical plaque control/anti-inflammatory agents) formed the basis of this consensus. RESULTS: Data support the belief that professionally administered plaque control significantly improves gingival inflammation and lowers plaque scores, with some evidence that reinforcement of oral hygiene provides further benefit. Re-chargeable power toothbrushes provide small but statistically significant additional reductions in gingival inflammation and plaque levels. Flossing cannot be recommended other than for sites of gingival and periodontal health, where inter-dental brushes (IDBs) will not pass through the interproximal area without trauma. Otherwise, IDBs are the device of choice for interproximal plaque removal. Use of local or systemic anti-inflammatory agents in the management of gingivitis has no robust evidence base. We support the almost universal recommendations that all people should brush their teeth twice a day for at least 2 min. with fluoridated dentifrice. Expert opinion is that for periodontitis patients 2 min. is likely to be insufficient, especially when considering the need for additional use of inter-dental cleaning devices. In patients with gingivitis once daily inter-dental cleaning is recommended and the adjunctive use of chemical plaque control agents offers advantages in this group.
Cutler, C. W., et al. (2000). "Clinical benefits of oral irrigation for periodontitis are related to reduction of pro-inflammatory cytokine levels and plaque." J Clin Periodontol 27(2): 134-143.
BACKGROUND: Although a growing body of evidence indicates that oral irrigation with water has therapeutic benefits in periodontitis, the mechanisms of action have not been elucidated. The aims of this study were: (1) to analyze the effects of oral irrigation (Water Pik Oral Irrigator) on the clinical signs of adult periodontitis (AP) and on the levels of interleukin-1 beta (IL-beta), prostaglandin-E2 (PGE2), interleukin-10 (IL-10) and interferon-gamma (IFN-gamma) in GCF, and (2) to analyze the influence of the periodontitis-related IL-1 genotype (IL-1GT) on these variables. METHOD: A single-center, blinded study in otherwise healthy humans (n= 52) with localized mild to moderate AP was carried out, using the following groups: group A (n= 12), no oral hygiene for 14 days; group B (n=20), routine oral hygiene (ROH) for 14 days; group C (n=20), supra-gingival oral irrigation plus ROH for 14 days. Group A patients were crossed-over to group C for 14 days (=day 28) after a professional prophylaxis. Group assignment was randomized by a coin toss, with the exception of group A subjects, who were self-selected as per recommendations of the internal review board for human subjects. GCF was sampled from 3 study teeth per patient and analyzed for IL-1 beta, PGE2, IL-10 and IFN gamma by ELISA on days 0, 7, 14 and 28. Probing pocket depths (PPD), clinical attachment levels (CAL), bleeding on probing (BOP), gingival index (GI) and plaque index (PI) were measured by a calibrated examiner (TWS) on days 0, 14 and 28. Analysis of covariance was performed using SAS 6.12 and Proc Mixed with group and IL-1GT as the factors and the baseline levels as the covariate, with output being least squares means and least significant difference (LSD). Significant differences were declared if the p-value for the F-statistic was < or =0.05. RESULTS: Oral irrigation plus ROH resulted in a significant reduction in PPD, BOP, GI and PI, as well as IL-beta levels by 7 days and PGE2 levels by 14 days, relative to ROH or no oral hygiene. Interestingly, decreased IL-1 beta levels in patients using oral irrigation plus ROH was accompanied by a trend for increased levels of the "anti-inflammatory" cytokine IL-10. ROH reduced GI, BOP and PI, and PGE2 levels by 14 days, but had no effect on IL-1 beta or IL-10 levels relative to no oral hygiene. The effects of no oral hygiene were reversed by a prophy followed by oral irrigation plus ROH for 14 days. No clinical differences were evident between IL-1 GT (+) patients (n= 1) and GT (-) patients (n=40), but the former had significantly elevated levels of GCF IL-10 and borderline increases in IL-1 beta (p=0.07). CONCLUSIONS: Oral irrigation with water for 14 days had an improved therapeutic benefit for AP over that of routine oral hygiene alone and this improvement was accompanied by a down-modulation of the pro-inflammatory cytokine profile in GCF.
Heo, S., et al. (2018). "Simplified nonsurgical treatment of peri-implantitis using chlorhexidine and minocycline hydrochloride." Journal of periodontal & implant science 48(5): 326-333.
PURPOSE: The present study investigated the outcomes of a newly-developed, simple, and practical nonsurgical treatment modality suitable for most forms of intrabony defects around failing dental implants using intrasulcular delivery of chlorhexidine solution and minocycline hydrochloride (HCl). METHODS: Forty-five dental implants in 20 patients diagnosed with peri-implantitis were included. At baseline and the study endpoint, the probing pocket depth (PPD), clinical attachment level (CAL), and the presence of bleeding on probing (BOP) at 6 sites around each implant were recorded. The radiographic osseous defect morphology at the mesial or distal proximal aspect of each implant was classified as 1) narrow or wide and 2) shallow or deep. For a comparative analysis of bone changes according to the defect morphology, the distance from the implant shoulder to the most coronal bone-to-implant contact point (DIB) at the mesial and distal aspects of each implant was measured at baseline and the endpoint. Patients were scheduled to visit the clinic every 2-4 weeks for intrasulcular irrigation of chlorhexidine and delivery of minocycline HCl. RESULTS: We observed statistically significant decreases in PPD, CAL, and BOP after treatment. At the endpoint, bone levels increased in all defects, regardless of the osseous morphology of the intrabony defect. The mean DIB change in deep defects was significantly greater than that in shallow defects. Although the mean bone gain in narrow defects was greater than in wide defects, the difference was not statistically significant. CONCLUSIONS: We propose that significant and sustainable improvements in both clinical and radiographic parameters can be expected when intrabony defects around dental implants are managed through a simple nonsurgical approach involving combined intrasulcular chlorhexidine irrigation and local delivery of minocycline HCl.
Prathapachandran, J. and N. Suresh (2012). "Management of peri-implantitis." Dental research journal 9(5): 516-521.
Peri-implantitis is a site-specific infectious disease that causes an inflammatory process in soft tissues, and bone loss around an osseointegrated implant in function. The etiology of the implant infection is conditioned by the status of the tissue surrounding the implant, implant design, degree of roughness, external morphology, and excessive mechanical load. The microorganisms most commonly associated with implant failure are spirochetes and mobile forms of Gram-negative anaerobes, unless the origin is the result of simple mechanical overload. Diagnosis is based on changes of color in the gingiva, bleeding and probing depth of peri-implant pockets, suppuration, X-ray, and gradual loss of bone height around the tooth. Treatment will differ depending upon whether it is a case of peri-implant mucositis or peri-implantitis. The management of implant infection should be focused on the control of infection, the detoxification of the implant surface, and regeneration of the alveolar bone. This review article deals with the various treatment options in the management of peri-implantitis. The article also gives a brief description of the etiopathogenesis, clinical features, and diagnosis of peri-implantitis.
Sälzer, S., et al. (2015). "Efficacy of inter-dental mechanical plaque control in managing gingivitis--a meta-review." J Clin Periodontol 42 Suppl 16: S92-105.
FOCUSED QUESTION: What is the effect of mechanical inter-dental plaque removal in addition to toothbrushing, on managing gingivitis using various formats of inter-dental self-care in adults based on evidence gathered from existing systematic reviews? MATERIAL & METHODS: Three Internet sources were searched by a strategy designed to include systematic reviews on inter-dental cleaning devices. Plaque and gingivitis scores were the primary parameters of interest. Characteristics of selected papers were extracted. The potential risk of bias was estimated and the acquired evidence was graded. RESULTS: Screening of 395 papers resulted in six systematic reviews. Two papers evaluated the efficacy of dental floss, two of inter-dental brushes (IDB), one of woodsticks and one of the oral irrigator. Weak evidence of unclear or small magnitude was retrieved that supported dental floss, woodsticks and the oral irrigator to reduce gingivitis in addition to toothbrushing. No concomitant evidence for an effect on plaque emerged. There is moderate evidence that IDBs in combination with toothbrushing reduce both plaque and gingivitis. CONCLUSION: Evidence suggests that inter-dental cleaning with IDBs is the most effective method for inter-dental plaque removal. The majority of available studies fail to demonstrate that flossing is generally effective in plaque removal. All investigated devices for inter-dental self-care seem to support the management of gingivitis, however, to a varying extend.
Waerhaug, J. (1976). "The interdental brush and its place in operative and crown and bridge dentistry." J Oral Rehabil 3(2): 107-113.
The effect of the interdental brush was evaluated on sixty-seven extracted teeth which were stained and examined under the stereomicroscope. Thirty-one of the teeth were totally covered with plaque when the interdental brush was used on them immediately before extraction. Thirty-six of the teeth were from patients who had used the interdental brush routinely for several years. The interdental brush was found to have an excellent effect both in the central part of the interdental space and on the embrasures. However, the most noteworthy finding was that it removes plaque as far as 2-2 1/2 mm below the gingival margin. This means that restorations can be kept free of plaque, even if they are extended into the pocket. In modern dentistry 'extension for prevention of dental caries' has become a controversial principle because subgingival restorations retain plaque which induces destructive periodontal disease. In many cases this problem can be solved by introducing the interdental brush.
